Abdulaziz AlQahtani 1, Nyall R London Jr 2 3 4, Paolo Castelnuovo 5, Davide Locatelli 6, Aldo Stamm 7, Aaron A Cohen-Gadol 8, Hussam Elbosraty 9, Roy Casiano 10, Jacques Morcos 11, Ernesto Pasquini 12, Georgio Frank 13, Diego Mazzatenta 13, Garni Barkhoudarian 14, Chester Griffiths 14, Daniel Kelly 14, Christos Georgalas 15, Narayanan Janakiram 16, Piero Nicolai 17, Daniel M Prevedello 2 18, Ricardo L Carrau 2 18Affiliations expand
- PMID: 32105301
- PMCID: PMC7047871 (available on 2021-02-27)
- DOI: 10.1001/jamaoto.2019.4864
Abstract
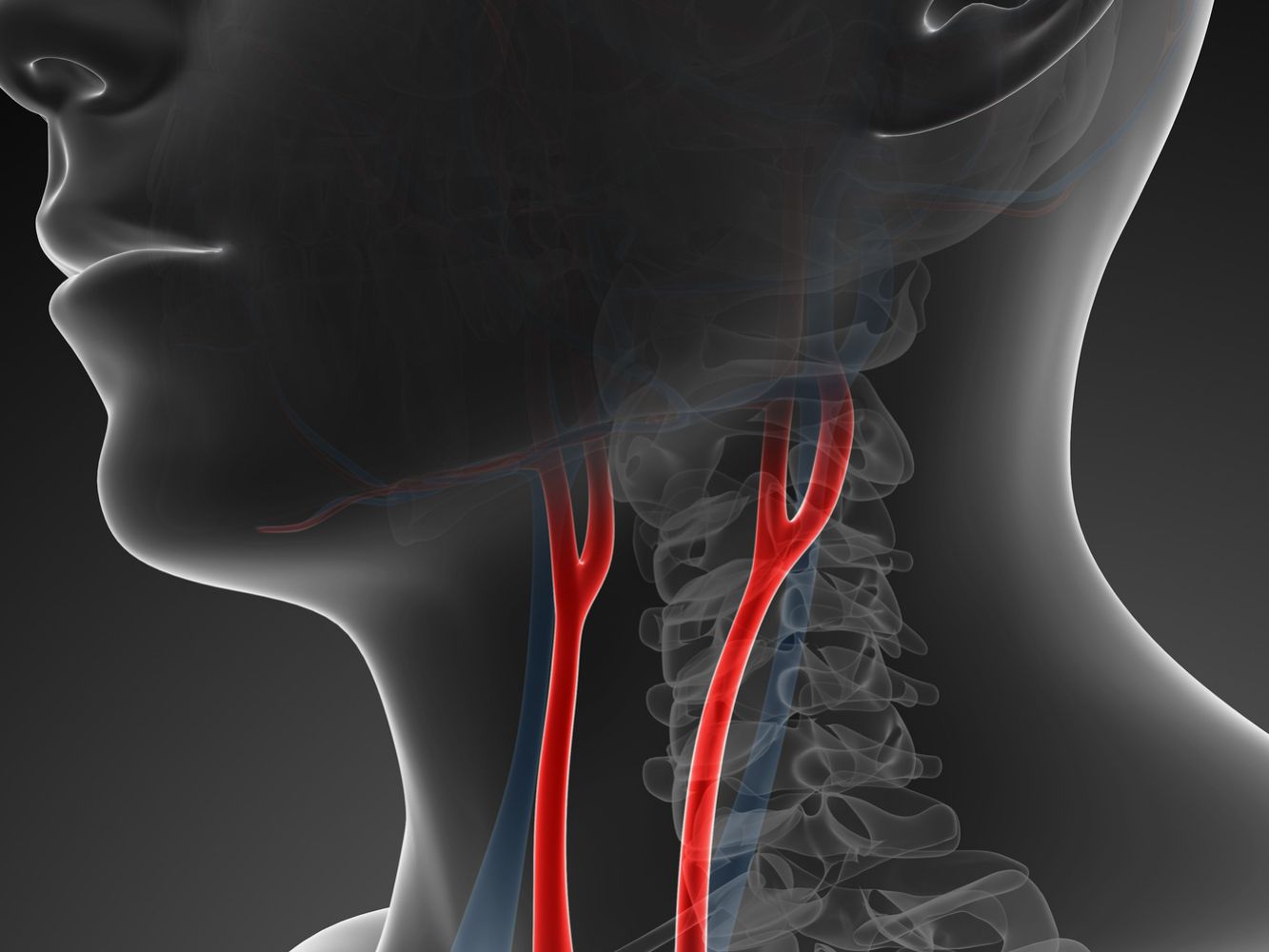
Importance: Injury to the internal carotid artery (ICA) during endoscopic endonasal skull base surgery does not typically occur as an isolated circumstance but often is the result of multiple factors.
Objective: To assess the factors associated with ICA injury in an effort to reduce its occurrence.
Design, setting, and participants: This quality improvement study used a multicenter root cause analysis of ICA injuries sustained during endoscopic endonasal skull base surgery performed at 11 tertiary care centers across 4 continents (North America, South America, Europe, and Asia) from January 1, 1993, to December 31, 2018. A fishbone model was built to facilitate the root cause analysis. Patients who underwent an expanded endoscopic endonasal approach that carried a substantial potential risk of an ICA injury were included in the analysis. A questionnaire was completed by surgeons at the centers to assess relevant human, patient, process, technique, instrument, and environmental factors associated with the injury.
Main outcomes and measures: Root cause analysis of demographic, human, patient, process, technique, instrument, and environmental factors as well as mortality and morbidity data.
Results: Twenty-eight cases of ICA injury occurred during 7160 expanded endoscopic endonasal approach procedures (incidence of 0.4%). The mean age of the patients was 49 years, with a female to male predominance ratio of 1.8:1 (18 women to 10 men). Anatomical (23 [82%]), pathological (15 [54%]), and surgical resection (26 [93%]) factors were most frequently reported. The surgeon’s mental or physical well-being was reported as inadequate in 4 cases (14%). Suboptimal imaging was reported in 6 cases (21%). The surgeon’s experience level was not associated with ICA injury. The ICA injury was associated with use of powered or sharp instruments in 20 cases (71%), and use of new instruments or technology in 7 cases (25%). Two patients (7%) died in the operating room, and 3 (11%) were alive with neurological deficits. Overall, patient-related factors were the most frequently reported risk factors (in 27 of 28 cases [96%]). Factors associated with ICA injury catalyzed a list of preventive recommendations.
Conclusions and relevance: This study found that human factors were associated with intraoperative ICA injuries; however, they were usually accompanied by other deficiencies. These findings suggest that identifying risk factors is crucial for preventing such injuries. Preoperative planning and minimizing the potential for ICA injury also appear to be essential.
Conflict of interest statement
Conflict of Interest Disclosures: Dr Casiano reported receiving ad hoc consulting fees from Medtronic, Olympus ENT, and MeilMed Inc outside the submitted work. Dr Barkhoudarian reported receiving personal fees from Vascular Technology Inc outside the submitted work. Dr Kelly reported receiving ad hoc consulting fees from Mizuho Inc outside the submitted work. Dr Prevedello reported being a consultant for Stryker, Medtronic, and Integra and receiving royalties from Mizuho and KLS-Martin. No other disclosures were reported.